Supporting people with an application on MHPSS, Cordaid does it in Yemen.

I would love to hear more about the MHPSS application that you are working on, but could you tell me first about the other projects that Cordaid is doing in Yemen?
Cordaid works with a network of local partners, we started in Yemen primarily focusing on health interventions supporting pregnant women and newborns. We’ve expanded to Humanitarian response in food security with cash for food, recovery of livelihoods, rehabilitation of health facilities and mental health services.
One of Cordaid’s key priorities is building strong relationships with local partners, working in equitable partnerships. Cordaid’s role is to provide access to funding, support joint monitoring and accountability and when needed add technical support, while empowering local organizations to lead. We believe locally led programs are more effective and local actors should have a leading role in programs in their own country.
Could you tell us a bit more about the current situation in Yemen?
The crisis in Yemen has been ongoing since 2015, and it will soon be 10 years. Unfortunately, there is no immediate solution in sight. While global attention is shifting to other crises, the situation here remains dire, with many people lacking basic support. The conflict is still very much alive, and families struggle to survive in a failing economy. Jobs are scarce, and infrastructure, such as electricity, is unreliable, with power cuts lasting more than 15 hours a day.
The conflict is still very much alive, and families struggle to survive in a failing economy.
Why did you decide to come up with an MHPSS program? What does that look like?
Because of the conflict, a lot of people have mental health or psycho- social problems. World Health Organization (WHO) states that one out of four people in Yemen needs mental health support. There is not enough support available since many organisations are focused on ‘filling the empty stomach’ ánd, people that are looking for mental support are being stigmatized – something that has to change. People who are looking for mental health support are seen as ‘evil’ by others in their communities – especially people who are still living in traditional villages or communities.
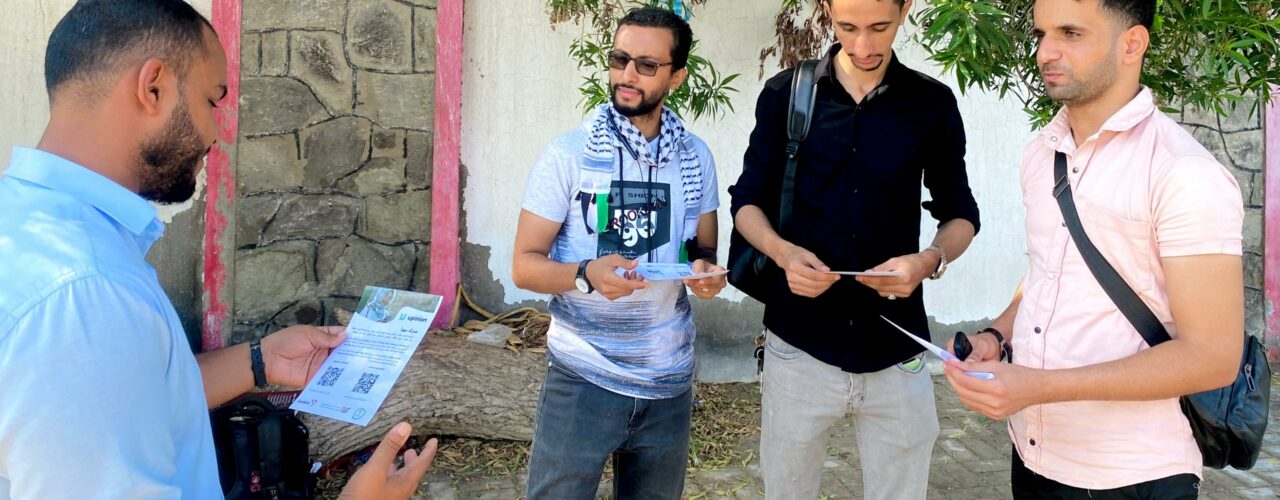
Our local partner and the government agreed on the fact that a MHPSS program would be a good idea and we started to write a project plan in which we would work closely together with the ministry of health and local partners. In the first phase of the project development we focused on gathering information and input from Yemini people. What do people need? Who do we want to serve? Who can we rely on for professional support? We organized discussion groups and did lots of online research to be able to create an important MHPSS online platform.

What are the challenges within this program?
The first challenge is internet access. Since the app is online-based, we are exploring ways to make it accessible with weak internet or even offline.
The second challenge is the social stigma surrounding mental health. People fear being labeled as ‘evil’ or ‘sick.’ We launched a radio campaign to raise awareness and reduce stigma, emphasizing that user privacy is protected and that their information will not be used for anything other than their well-being.
Another challenge is to organise and cover the costs for referrals to specialised care for those using the app and are in need of more specialized support. Also qualified staff that can provide these mental health services are scarce.
Lastly, securing long-term funding is challenging, as it’s difficult to quantify the project’s impact. Mental health outcomes are often complex and take time to manifest, making it harder to demonstrate immediate results.
Is the whole program via an app?
Yes, the app provides essential information on managing stress and anxiety and includes a service directory to help users find mental health resources nearby. For those in remote areas, we offer the option to reach out for a consultation or referral through the app. Additionally, the app includes games, self-assessments, podcasts, and videos to cater to users with different literacy levels. One of our key features is a ‘question box’ where users can submit questions, fostering a sense of community and peer support. We also plan to implement a hotline staffed by social workers and mental health professionals to provide real-time assistance. Socials workers and specialized staff will be there to listen to people and provide them with advice and support if needed.
What is your target group? Who do you expect to find you?
Our target audience primarily includes women, that face more challenges and mental pressure in life due to cultural norms and restrictions, and young people, as they are more likely to use technology. The older generation may be less familiar with using apps, but we hope that through awareness campaigns and word-of-mouth, we can reach as many people as possible, especially those in remote areas who don’t have easy access to mental health services.
What is your hope for this project?
I hope the app becomes a valuable tool for people in remote areas. Our goal is to scale up the project once users discover its benefits. Additionally, I hope that the app will be managed locally, with partners and the community playing a central role. Without local involvement, the project won’t be sustainable.
Without local involvement, the project won’t be sustainable.
What is your wish for the people who are searching for help?
I hope people who use the platform will find the support they need. I want the app to help normalize seeking mental health support, guiding users toward professional services or community resources before problems escalate. We aim to provide a space where people feel safe and understood and can access help when they need it.
I hope people who use the platform will find the support they need.
Is there anything else you would like to share?
I hope the app will be a great success and that it can be implemented in other areas to support those suffering from similar mental health challenges. We are still refining the app and will use the next six months to focus on design and user experience. After that, we’ll scale up based on user feedback to ensure we offer the best possible support. We’ll notify everyone when the app is ready to launch!

The web app is developed with innovation funding of the Dutch Relief Alliance (DRA)
Do you want to read more about the work of Cordaid? Click here.
Author: Marianne van Elst-Sijtsma
Date: 11th of October 2024


